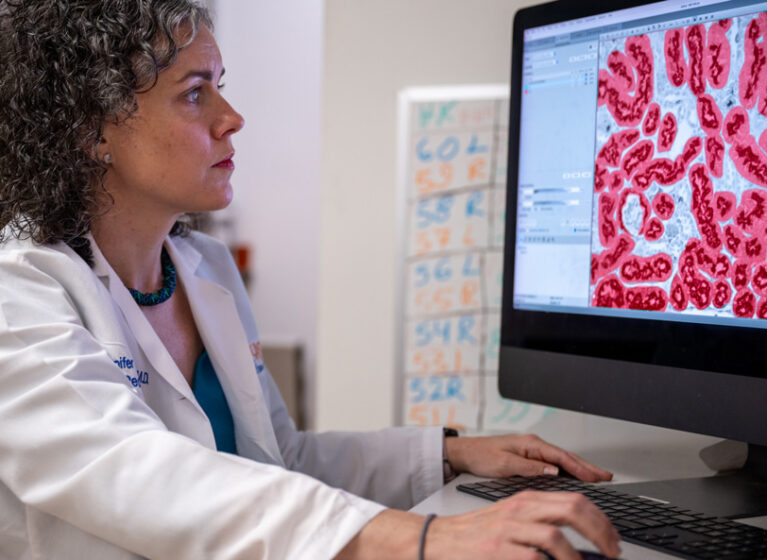
A recent study showed that over half of children born between 24-28 weeks of gestation had kidney health issues at 2 years old. These problems included abnormal kidney function, protein in their urine, and high blood pressure. At UVA Health Children’s, Jennifer Charlton, MD, associate professor in the division of pediatric nephrology, researches the pathways that link preterm birth and long-term kidney health. A better understanding of these pathways could create immediate clinical outcome improvements.
“What we don’t know is if you are born early, do you continue to make nephrons for the same amount of time as a fetus would? And are they as healthy?” says Charlton. “However, we do know that chronic kidney disease is relatively common in preterm babies. We are working to understand the mechanisms of how being born early leads to developing CKD.”
Clinical Impacts of Prematurity on Kidney Health
Using preterm and full-term mice, Charlton and colleagues found variations in gene expression that led to changes in the vitamin D metabolic pathway. These genes include those that regulate the conversion of hydroxyvitamin D to dihydroxyvitamin D, a process that occurs in the kidneys. In the preterm mice, the enzymes for this metabolism were downregulated.
Humans have a wide variation in glomerular endowment (also called nephron endowment). Nephron numbers can range from 200,000–2,700,000, which are present from birth. While mice models are imperfect for comparing glomerular endowment (mice produce some nephrons after birth), this research offers a promising model for understanding the impact of nephron number on these metabolic pathways. This research may prove critical for premature babies, as there is an association between vitamin D deficiency and other common conditions of prematurity, such as bronchopulmonary dysplasia and retinopathy of prematurity.
Charlton and her team received a grant to continue expanding their understanding of the vitamin D pathway in this preterm mouse model based on this preliminary data. This includes testing the hypothesis that supplementing vitamin D could improve the health of the developing kidney and that maternal vitamin D deficiency may play a role in the pathogenesis of CKD in those born preterm.
“I’m excited to work out this pathway because if it is true that preterm babies have inadequate conversion of vitamin D, then that could be a therapeutic target,” says Charlton. “In general, patients with advanced CKD cannot convert 25 vitamin D to the active form of 1,25 vitamin D. These patients receive 1,25 vitamin D to treat the complications of metabolic bone disease. If we validate that preterm infants also cannot effectively activate vitamin D, we can potentially help the kidneys and other organs develop normally and naturally by supplementing active vitamin D.”
Building on Kidney-Research Breakthroughs
Charlton credits much of her success to two “game-changing” NIH workshops she attended, including one on glomerular morphometrics. This workshop and its resulting collaborations enabled Charlton to leverage new research on noninvasive ways of measuring nephron number. With two R01 grants for this research, Charlton and long-time collaborator Dr. Kevin Bennett have focused on mouse studies to expand the use of contrast agents to look at nephron number, including nephron endowment, in different ways – a critical step in evaluating kidney health in preterm newborns.
The second NIH workshop focused on neonatal acute kidney injury. This workshop led to research showing that 30% of critically ill neonates had an acute kidney injury during their NICU stay. The Neonatal Kidney Collaborative (NKC) was founded after this workshop highlighted so many critical knowledge gaps. The mission of the NKC is to improve the health and well-being of newborns with or at risk for kidney disease through multidisciplinary collaborative research, advocacy, and education. The NKC has members from around the world and has published over 20 manuscripts on the prevalence and associations of acute kidney injury in neonates, including:
- Fluid overload
- Hypertension
- Caffeine
The NKC also hosts a family council to engage premature children and their families in ongoing research. Currently serving a term as vice president, Charlton was elected to become president of the collaborative in 2025.
Creating Pathways to Help Babies Thrive
UVA Health Children’s has built a structure that accelerates the research of Charlton and others. That includes a highly collaborative NICU that supports neonatal research. Robust support from basic sciences including the Children’s Health Research Center, statistical support through public health, and talented trainees in the PICU and NICU have helped accelerate research through the integration of clinical care, education, and research.
“I also benefit from the infrastructure in my division, where my partners allow me protected time to do research,” says Charlton. “These research efforts are marathons, not sprints, and their consistent support is a huge help to empowering my research.”
Trained as a pediatric nephrologist, Charlton was not initially interested in research until she saw how much opportunity there was to improve the lives of her patients through better universal understanding of the conditions she was treating.
“One-in-10 babies are born preterm. This is not an uncommon problem,” says Charlton. “We’ve made a huge evolution in medicine: We can help babies born at 22 weeks to live, but there is still morbidity associated with it. Now that the mortality of preterm birth has decreased, it is time to improve the morbidity and help these babies to thrive, not just survive.”