Recent UVA Health research could eventually transform how we treat heart attacks. By studying a key enzyme called DYRK1A, Matthew J. Wolf, MD, and his team of researchers have found a way to stimulate heart cells to regenerate after a heart attack.
This breakthrough offers hope for new therapies that could repair damaged hearts and prevent long-term complications following a myocardial infarction.
“By inhibiting the DYRK1A kinase, we promote cardiomyocyte cycling and regeneration. Mice lacking this kinase or treated with inhibitors showed improved heart function and an upregulation of genes associated with cell cycling and regeneration,” notes Wolf.
Why Target DYRK1A?
DYRK1A (dual-specificity tyrosine phosphorylation-regulated kinase 1A) is an enzyme that regulates how cells grow and divide. In adult hearts, cells called cardiomyocytes rarely divide, making it difficult for the heart to repair itself.
"The vast majority of cells that re-enter the cell cycle after a heart attack are not myocytes but fibroblasts and other cells that lead to scarring. Cardiomyocyte regeneration is a very low-abundance event, occurring rarely," says Wolf.
With the loss of cardiomyocytes, the heart can weaken over time following an injury like a heart attack. This can lead to heart failure.
"We analyzed the genes expressed in young versus older mouse hearts and identified DYRK1A as a potential candidate that acts as a brake on cycling in adult cardiomyocytes," says Wolf. The research team focused on lifting the “brakes” that stop cardiomyocytes from dividing.
Studying the Role of DYRK1A in Heart Cell Regeneration
To explore DYRK1A’s role in cycling, the team used two approaches:
- Genetic modification: They engineered mice lacking DYRK1A to observe how this affected the ability of their heart cells to regenerate.
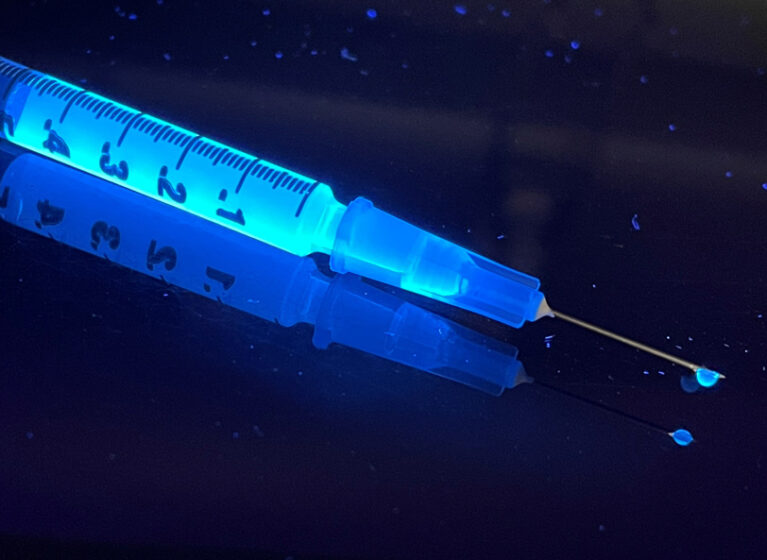
- Pharmacological treatment: They treated a different group of mice with harmine, a plant-based compound, to block DYRK1A’s activity.
By tracking cardiomyocyte division with advanced imaging technology, they discovered that inhibiting DYRK1A significantly improved heart cell regeneration and heart function after a heart attack. “In mice where DYRK1A was knocked out specifically in cardiomyocytes, we observed significant improvements in heart function and increased regenerative activity after myocardial infarction.”
Harmine: A Potential Key Ingredient in Heart Healing
A natural compound found in plants used in some traditional medicines, harmine, played a crucial role in the study. Harmine was shown to allow heart cells to regenerate in greater quantities after a heart attack than without it. Wolf says, "The harmine itself binds to the active site of the kinase and prevents it from being catalytically active."
The team also observed that these regenerating heart cells secreted helpful proteins, known as paracrine factors, which possibly supported further healing. "I think these cells that are trying to divide are also expressing paracrine factors that permeate the local microenvironment of the heart and improve heart function. By identifying these factors, we could potentially use them as a therapy in the future,” notes Wolf.
Addressing Safety Concerns
A major concern with encouraging cell division is the risk of cancer. The research team addressed this by carefully monitoring for signs of uncontrolled cell growth.
They found no evidence of tumors in their studies. "We didn’t see any evidence of tumor proliferation in this study, partly because of the short usage, where mice received the drug for only a week, once a day."
“The cycling of those cardiomyocytes induced by this inhibitor is context-dependent, meaning that you have to have an injury for the drug to have an effect. We get very little proliferation in uninjured mice," Wolf explains.
Promising Results
The findings were significant for further research and possible future development of a new therapy to use during heart attack care. “The heart function improved by about twofold in the harmine group compared to the non-treated group," says Wolf.
Specifically, the harmine-treated mice experienced only a 15-20% decline in heart function after a heart attack, compared to a 40% decline in untreated mice.
DYRK1A Inhibition: What’s Next?
“This research is just the beginning,” Wolf says. “The road to clinical applications is long, but we’re optimistic about the possibilities.” Wolf and his team are already planning the next steps, including:
- Developing more precise DYRK1A inhibitors to improve safety
- Studying the detailed biology of cardiomyocyte cycling to optimize treatments
- Investigating how this approach could complement existing heart attack therapies
This discovery could transform how we treat heart attacks. By unlocking the heart’s ability to heal itself, researchers are working toward a future where injury from heart attack can be healed to a much greater extent than what's possible with current therapies.