Undernutrition is one of the largest global challenges affecting child health. While most commonly associated with insufficient consumption, undernutrition also occurs when nutrients can’t be effectively used. Infections and inflammation in the gut can disrupt digestion and prevent the body from absorbing what it needs. In 2022, more than 200 million children were suffering from the effects of undernutrition, according to the World Health Organization (WHO).
The immediate consequences of undernutrition are apparent. Undernutrition is a contributing factor in half of all deaths in children under the age of 5. There are also long-term consequences for survivors of undernutrition in early childhood. These consequences include reduced growth, immune dysfunction, and effects on cognitive development.
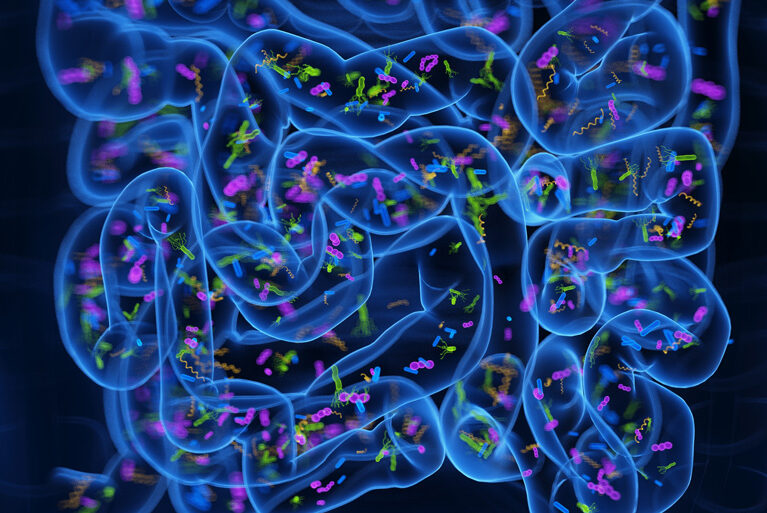
Early childhood is a foundational period of development. This includes the development of the gut microbiome, which can affect growth and immunity. Research suggests these microbiome changes may have ripple effects through generations.
A new model developed by UVA Health Children’s researcher Carrie Cowardin, PhD, and her colleagues offers a new perspective. It shows promise for helping scientists better understand the role of gut microbes passed from parents to children. It also shows how those inherited microbiomes affect childhood growth and immune system development.
Understanding the Impact of Intergenerational and Early Life Microbe Exposure
Traditionally, scientists transfer human microbiome samples into lab mice to study their impacts. Cowardin and her fellow researchers found it’s more effective to introduce the microbes to parent mice. Parents pass their microbes to their offspring at birth, allowing young mice to grow and develop their immune system along with these microbes. According to their study, which was recently published in the journal Microbiome, this “intergenerational colonization” more closely resembles the effects of undernutrition in early childhood.
Cowardin and her co-authors wrote: “Our results suggest intergenerational colonization with human microbiota samples is a useful approach with which to investigate microbiota-dependent changes in growth and immunity in early life.”
Cowardin, whose background is in infectious disease and immunology, has focused her research on how the gut microbiota during pregnancy and early postnatal life set the stage for lifelong immune responses. Understanding that the gut microbiome plays a pivotal role in shaping the development of both intestinal and systemic immune responses — and that undernourished children are known to have altered microbial communities and mucosal immunity — she developed a model of intergenerational growth stunting using human intestinal microbiota.
Parental Microbiome Contributes to Lifetime Health
“My colleagues and I wanted to look at how the timing of exposure to microbes influenced outcomes,” she says.
Cowardin and her colleagues tried first to use the mouse-model to understand the effects of maternal undernutrition on the gut microbiome. This had some unexpected consequences. “We actually had difficulties getting the mice to breed when we malnourished the mothers,” Cowardin says.
Fortunately, mice readily share microbiomes when housed together. So, the team had an additional avenue. “We malnourished the fathers,” she shares. “And then we added the mothers in. After 2 weeks, the mothers had a very similar microbiome.”
The resulting offspring had similar effects to those seen in human children: stunted growth and weakened immune systems.
“The composition of the microbiota during an early-life window seems to dictate immune outcomes,” Cowardin says. “I think the finding that it’s influencing immune development in a way that has persistent effects tells us how important that early-life window is.”
Translational Uses of This Model
On the translational side, Cowardin points to a reaffirmation of past studies. “Whether we’re taking microbiota from a healthy or stunted donor impacts both growth and immunity, which reinforces what we’ve seen before — that the composition of someone’s microbiome is related to growth. Our study illuminates changes to the immune system as well.”
Using this model will allow scientists to test potential treatments to boost immune function and protect children from infectious diseases, which can also help improve growth.
Still, Cowardin says, it’s something of a chicken-and-egg situation. “Does someone have disrupted gut microbiota because of infections with intestinal pathogens? Or did they get the infection because their microbiota is disrupted? We don’t fully understand the answer to these questions.”
The Microbiome’s Role in Precision Medicine
Cowardin runs an independent lab at UVA Health Children’s Child Health Research Center and is a member of the TransUniversity Microbiome Initiative (TUMI), which serves as UVA Health’s central hub for cutting-edge microbiome research.
She says she hopes to use the new model to better understand the role of the microbiome and, eventually, overcome some of the challenges children with undernutrition face. Including higher rates of infection and changes in cognitive development.
“We’re right on the cusp of understanding the consequences of the microbiome’s activities,” she says. “There’s a big push toward precision medicine these days, and the microbiome is actually a major component of that push. There can be huge variability between individuals that might require more tailored treatments.”
Cowardin adds: “Moving forward we’re thinking about how we can target these treatments to better improve quality of life and developmental outcomes with the ultimate goal, of course, of promoting healthy growth.”
For instance, Cowardin says she’s interested in targeting dietary therapies to different life stages to determine which has the greatest benefit — and then figuring out which microbes are causing the difference.
“What are the microbes doing?” she says. “Can we disrupt those harmful activities? Or boost beneficial bacteria? The model we developed can help us answer those questions.”
Cowardin also envisions using the new model to study whether dietary interventions could be customized to a certain part of the world rather than used as blanket therapies.
“I think, more and more, it’s looking like our interventions may need to be regionally specific,” she says. “Eventually, I believe the field will move toward recognizing individual differences once we have a better understanding of the needs of subpopulations of patients.”