Gastric varices (GV) are a rare but dangerous complication of portal hypertension. UVA Health is just one of a few centers in the U.S. treating GV with cyanoacrylate injections. This gluing procedure works where other approaches fail.
Another innovation: GV treatment teams bring together gastroenterology/hepatology specialists and interventional radiologists. This collaborative approach widens the range of treatment options for GV and allows for customization critical for addressing this condition.
Finding ways to customize and expand treatment options has set UVA Health apart as a leader and tertiary referral center for gastric varices.
Stomach vs. Esophageal Varices: Evaluated & Treated Differently
A majority of patients with portal hypertension (85%) develop esophageal varices (EV) — the most common cause of upper gastrointestinal bleeding. In most patients, varices in the columnar esophagus respond favorably to either endoscopic banding or transvenous intrahepatic portosystemic shunt (TIPS) insertion.
“Esophageal varices are the same in everybody,” says Zachary Henry, MD, associate professor of gastroenterology and hepatology. “We can treat all esophageal varices the same way, regardless of what causes them.”
Not so with GV. Because the vascular anatomy of the stomach varies among patients, no single therapy stands out as the best option for GV. Instead, the right approach relies on individual factors, including:
- The level of pressure in the veins
- Whether the varices are bleeding
- The presence of comorbid conditions, such as EV or ascites
“Gastric varices resemble a puddle, with multiple routes of blood inflow,” Henry says. “In this regard, they are very different from esophageal varices. While there are some overlaps in the initial management of both problems, ultimately, these are two very different phenomenon."
An Uncommon but Dangerous Complication
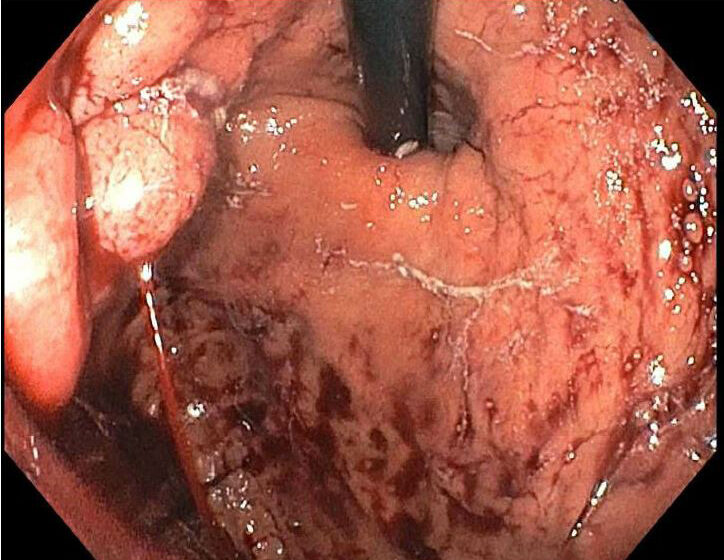
GV affect up to 25% of patients with portal hypertension, usually in those with cirrhosis of the liver. These dilated blood vessels in the stomach form under increased pressure in the “portal” system of veins that run through the stomach, pancreas, spleen, and intestines to the liver.
They are fragile and may bleed rapidly, putting patients at risk of dying if not treated quickly. Which is why, Henry says, "It's so important to classify them correctly and think about the patient’s anatomy and physiology when we're talking about management.”
Gluing Gastric Varices
GV bleeding is rare, and many gastroenterology/hepatology specialists are not well-trained in the endoscopic management of this condition. Our hepatologists offer a unique therapy for GV: endoscopic cyanoacrylate injection (ECI). This approach is not widely available at U.S. hospitals; however, it has proven effective for patients who are not candidates for interventional radiology procedures such as TIPS or balloon-occluded retrograde transvenous obliteration (BRTO).
According to a recently published article co-authored by Henry, “Since it was introduced in the 1980s, ECI has been shown to be effective at preventing both early and late rebleeding, with fewer complications compared with alcohol-based sclerotherapy or band ligation. Therefore, we recommend that ECI be considered the only definitive endoscopic therapy for cardiofundal GV.”
How Does the Procedure Work?
ECI requires two specialists working in tandem — one who guides the endoscope and syringe, and the other who injects glue into the vein. The adhesive polymerizes within a matter of seconds, obliterating the varices. Often, injection is necessary in multiple locations. Eventually, the glue is pushed back into the stomach and is excreted from the body with other waste.
“Communication and teamwork are key to making sure we adequately treat the varices without causing bleeding or other complications,” Henry says.
The patient is checked again in a month, and if necessary, the procedure is repeated until all varices are gone. Following data collected over the past 20 years, our specialists have increased the amount of glue injected during the initial procedure in hopes of reducing the number of follow-up procedures required.
“While we inject significantly more volumes of glue into each varix than other centers that offer this procedure, our results are essentially the same,” Henry says. “Our complication rates are low, and patients undergo fewer procedures.”
Why a Multidisciplinary Approach is Best
Patients with GV are best managed by a collaborative, multidisciplinary team that incorporates the expert perspectives of hepatologists, interventional radiologists, and interventional endoscopists. As a tertiary referral center for GV, our specialists carefully evaluate each patient to determine which technique would offer the best results.
“UVA Health offers multiple treatment options for managing GV that that can be tailored to each individual patient and their unique vascular anatomy,” says Stephen Caldwell, MD, professor of gastroenterology and hepatology. “There aren’t many medical centers in the country with the ability to do that. We can really find the right therapy ensuring the best outcomes possible.”