More than a decade ago, UVA Health neurosurgeon Jeffrey Elias, MD, pioneered focused ultrasound — a sound wave treatment now FDA-approved to treat essential tremor, Parkinson’s, and more.
Around the same time, UVA biomedical engineer Richard J. Price, PhD, began researching how different forms of focused ultrasound could boost cancer immunotherapy and enhance drug delivery to brain tumors.
Price’s work led to more innovation. Building on his work, UVA Health surgeons Craig Slingluff, MD, and David Brenin, MD, developed the world’s first clinical trials combining focused ultrasound with immunotherapy and chemotherapy to treat breast cancer and melanoma.
From these early investigations, several new clinical trials and research directions emerged to again position UVA Health as the world leader in focused ultrasound — this time in cancer immunotherapy.
What You Need to Know About Focused Ultrasound’s Potential in Cancer Treatment
About three years ago, UVA Health teamed up with the Focused Ultrasound Foundation to launch a first-of-its-kind Focused Ultrasound Cancer Immunotherapy Center. The center is headed by Price, Slingluff, and Brenin.
In this Q&A, the three codirectors share how focused ultrasound is becoming a game-changer for cancer and what to watch for next.
How did research into using focused ultrasound for cancer begin?
Price: The earliest treatments of cancer with focused ultrasound centered on its ability to thermally ablate tumor tissue. It was developed as an alternative to radiation treatments, with the potential to offer unlimited treatments because the energy deposition is non-ionizing.
We have learned that the thermal ablation component is useful for neoplasms like uterine fibroids and breast fibroadenoma. But for the treatment of metastatic disease, the thermal ablation needs to be combined with immuno- or chemotherapy. The Mel70 trial, as we originally dubbed it, is designed to leverage the influence of heat shock on tumor tissue to make immunotherapy more effective.
Where does the research stand today?
Price: Research is expanding exponentially, with most of the effort in drug delivery to brain tumors. At UVA Health, we are centered on combining focused ultrasound with immunotherapy, but there will be other strategies on the horizon.
Many clinical trial papers have been published. There are thousands of pre-clinical studies published.
What other trials are underway or poised to begin at UVA Health?
Price: There is a trial underway that uses focused ultrasound for another mode of action — sonodynamic therapy of brain tumors.
Another for advanced melanoma combines focused ultrasound with immune therapy.
One coming on the horizon will use focused ultrasound to, hopefully, improve a T cell therapy, known as bispecific armed T cells (BATS), for glioblastoma.
What are the most exciting potential applications for focused ultrasound in cancer treatment?
Price: For immunotherapy, the hope is that focused ultrasound will convert immunologically cold tumors into hot tumors that respond to immunotherapy.
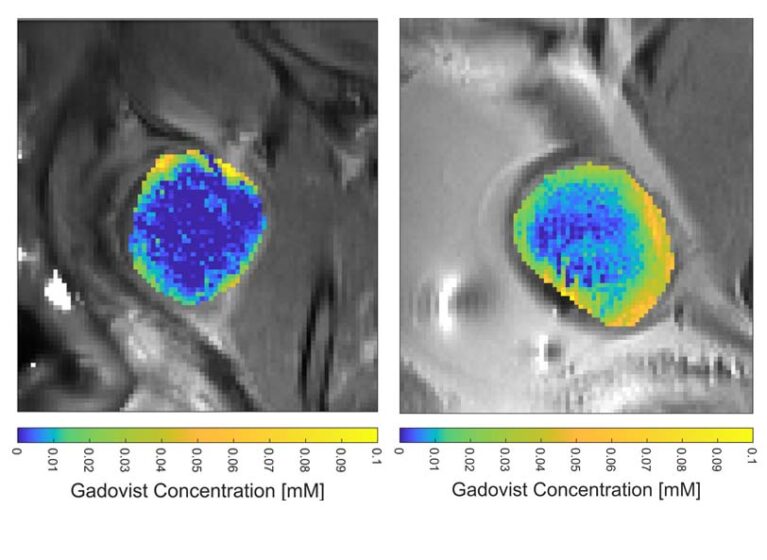
There are also emerging applications wherein focused ultrasound is used to improve drug delivery by enhancing the delivery of nanoparticles to brain tumors. This could change the treatment of these patients by having a regular focused ultrasound application when they receive their chemotherapy infusions.
My lab is working on using focused ultrasound to improve gene delivery to tumors, including CRISPR Cas9 genome editing of tumors, to improve their response to other therapies.
We are also exploring how advanced MRI techniques can be used to measure responses in brain tumors to focused ultrasound drug delivery.
Another very exciting new development is a mechanical ablation modality known as histotripsy. It has the potential to destroy tumors and leave a strong immunological signature that can be combined with immunotherapies.
Could you expand on how focused ultrasound helps overcome immunotherapy’s limitations?
Price: We have learned that focused ultrasound improves the flow of tumor antigen to draining lymph nodes, which means there is a higher probability that the immune system will recognize the cancer and mount a better immunological response. We have very compelling data to this effect and hope to use it soon to design better combination therapies.
Slingluff: Our colleague, Patrick Dillon, MD, is leading a clinical trial that grew out of UVA Health science on combining focused ultrasound with a chemotherapy agent with immune-modulating properties, where mice treated with the combination had better control of breast cancers and longer survival.
We’re excited to be offering histotripsy for liver tumors, and to design new clinical trials combining it with immune therapy.
What’s next on the horizon for focused ultrasound in cancer treatment?
Brenin: It is our hope that focused ultrasound therapies will allow the recent successes of immunotherapy in the treatment of some cancers to be applied more broadly. At this time, cancer immunotherapy is very successful at treating some cancer patients, but not most.
Focused ultrasound therapies may enhance the effectiveness of immunotherapies, allowing these treatments to benefit a much larger group of patients with different types of cancers.
Price: Two treatment modalities going through an exponential growth phase are, as noted above, blood-brain barrier opening with focused ultrasound for brain tumor treatment and mechanical ablation of solid tumors with histotripsy. We are hopeful the latter will be paired with immunotherapies more commonly soon.
I hope that, further down the road, we will see focused ultrasound paired clinically with more advanced delivery vehicle strategies, including gene therapies and even genome editing.
We and others have shown that focused ultrasound can markedly augment the delivery of lipid nanoparticles to brain tumors. Hopefully, this type of strategy can be pushed into clinical trials soon.