
Continuing advances in medical technology have resulted in the pioneering and evolution of minimally invasive techniques to treat valvular and structural heart disease. “Transcatheter therapy has revolutionized how we care for patients,” says structural and interventional cardiologist Nishtha Sodhi, MD. “It allows us to care for more complex patients, including those who may otherwise be turned down for surgery due to their age or co-morbidities.”
Examples of these minimally invasive technologies include:
- Transcatheter aortic valve replacement (TAVR)
- MitraClip for the repair of the leaky regurgitant mitral valve
- Transcatheter replacement of the mitral, tricuspid and pulmonic valves
- Repair of the tricuspid valve
- Closure of small holes in the heart (ASD/PFO) that are implicated in stroke
- Watchman device for the closure of the left atrial appendage, implicated in stroke
- Clinical trial devices for the left ventricular muscle in congestive heart failure patients
TAVR: UVA on the Forefront
The UVA Advanced Cardiac Valve Center has been performing TAVR since it was first introduced in 2009; it was one of the first 26 U.S. sites selected to participate in the initial PARTNER (Placement of Aortic Transcatheter valve) trial. Since 2014, UVA has completed more than 1,000 valvular and structural heart procedures.
With greater volumes come greater skill and greater exposure to a variety of cases. Below is one example of a complex case with a positive outcome made possible by the collaborative efforts of a multidisciplinary heart team that includes interventional cardiologists, cardiac surgeons, imaging specialists, nurse practitioners, nurses and many others.
“Our team works together to comprehensively evaluate patients and design a unique treatment strategy that meets the personalized needs of every patient and family,” says Dr. Sodhi. “The patient is always the focus at UVA – we advocate for and ensure that patients and their families feel at ease in all aspects of their care.”
Case Study: Cardiac Arrest Treated with Emergent Stents and TAVR While on Mechanical Support with ECMO and IABP
Patient: 88-Year-Old Male
The patient was transferred to UVA with difficulty breathing. He was healthy, with no prior major medical issues or diagnoses.
Evaluated By: Structural and Interventional Cardiologist Nishtha Sodhi, MD, and Cardiac Surgeon Kenan Yount, MD, MBA
Diagnosis: NSTEMI, Severe Aortic Stenosis, Coronary Artery Disease and Acute Decompensated Systolic Congestive Heart Failure
The patient had multiple diagnostic tests, including an echocardiogram of the heart. The aortic valve, the main valve allowing blood to flow out of his heart to the body, was severely blocked. His heart muscle function was very weak and he was in acute decompensated congestive heart failure. His heart muscle and blood work suggested that he had an acute heart attack from artery blockage.
“This was a guy who went from being healthy and taking hardly any medicines to being acutely critically ill,” says Dr. Sodhi. “It’s more common for people to present with symptoms sooner, but we do get some patients who come in and they’re quite advanced in the disease process. Sometimes patients don’t have any symptoms or they don’t have the classic cardiac symptoms, causing the heart condition to go undetected.”
Treatment: Emergent Stent Placement and TAVR on ECMO and IABP Mechanical Support
“My cardiac surgery colleague, Dr. Kenan Yount, and I had an extensive discussion with the patient and his family, and we decided to treat him minimally invasively rather than with traditional open-heart surgery,” says Dr. Sodhi.
During his evaluation, the patient’s heart and lungs stopped and he required resuscitation. He was emergently placed on an ECMO (extra-corporeal membrane oxygenation) machine and an Intra-Aortic Balloon Pump (IABP) to support his heart and lungs. This mechanical support is what provided blood circulation and oxygenation to his body.
Dr. Sodhi then emergently placed stents in two of his major heart arteries, the left anterior descending (LAD) and circumflex arteries, effectively restoring blood flow. “A CT of the head was normal and once the patient got to the ICU he was moving all four extremities and demonstrated that his neurological status was intact, which allowed us to move on to the next stage of his treatment,” says Dr. Sodhi
The next morning, the TAVR procedure was performed while the patient remained on ECMO. “We sized the TAVR valve by transesophageal echocardiogram and placed the new aortic valve via his femoral artery,” says Dr. Sodhi. “We obtained an excellent valve result and decided to keep the ECMO support in for the next few days to allow the patient’s heart muscle and hemodynamics to recover from all of the acute cardiac issues.”
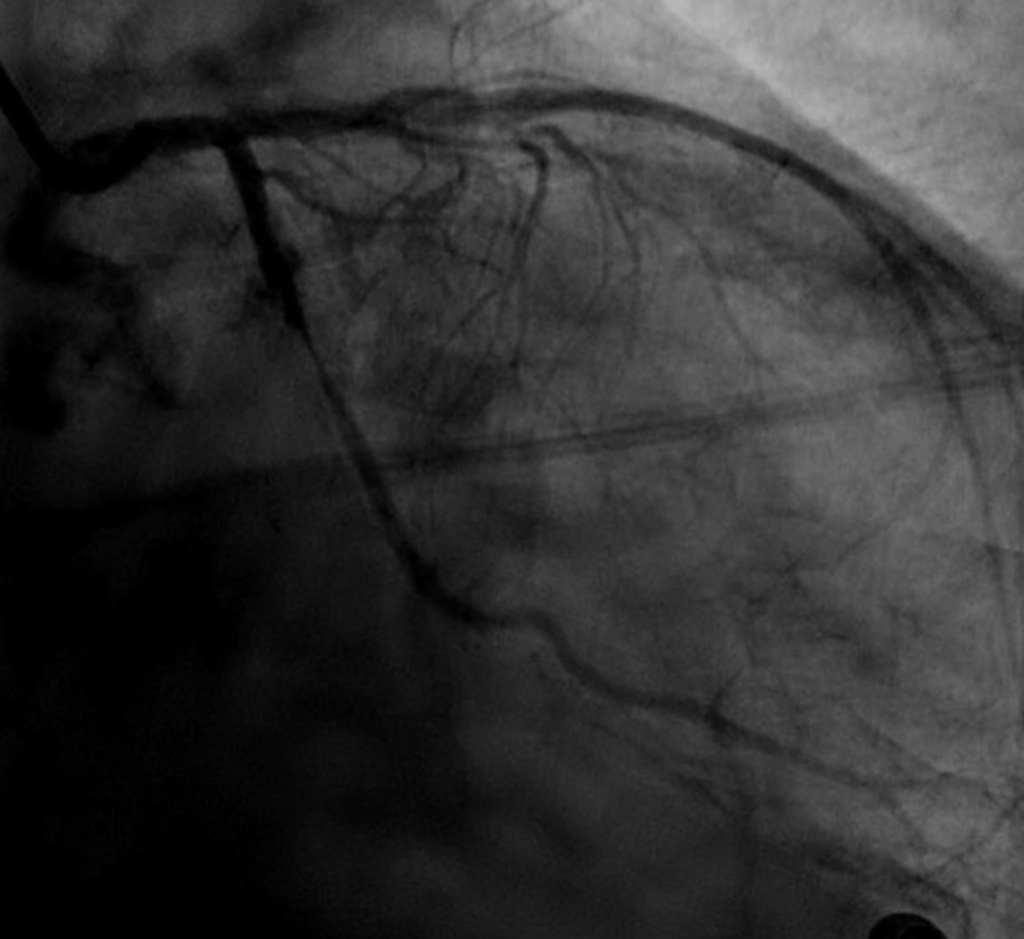
Circumflex artery prior to stenting 
Circumflex artery post-stenting 
LAD artery prior to stenting 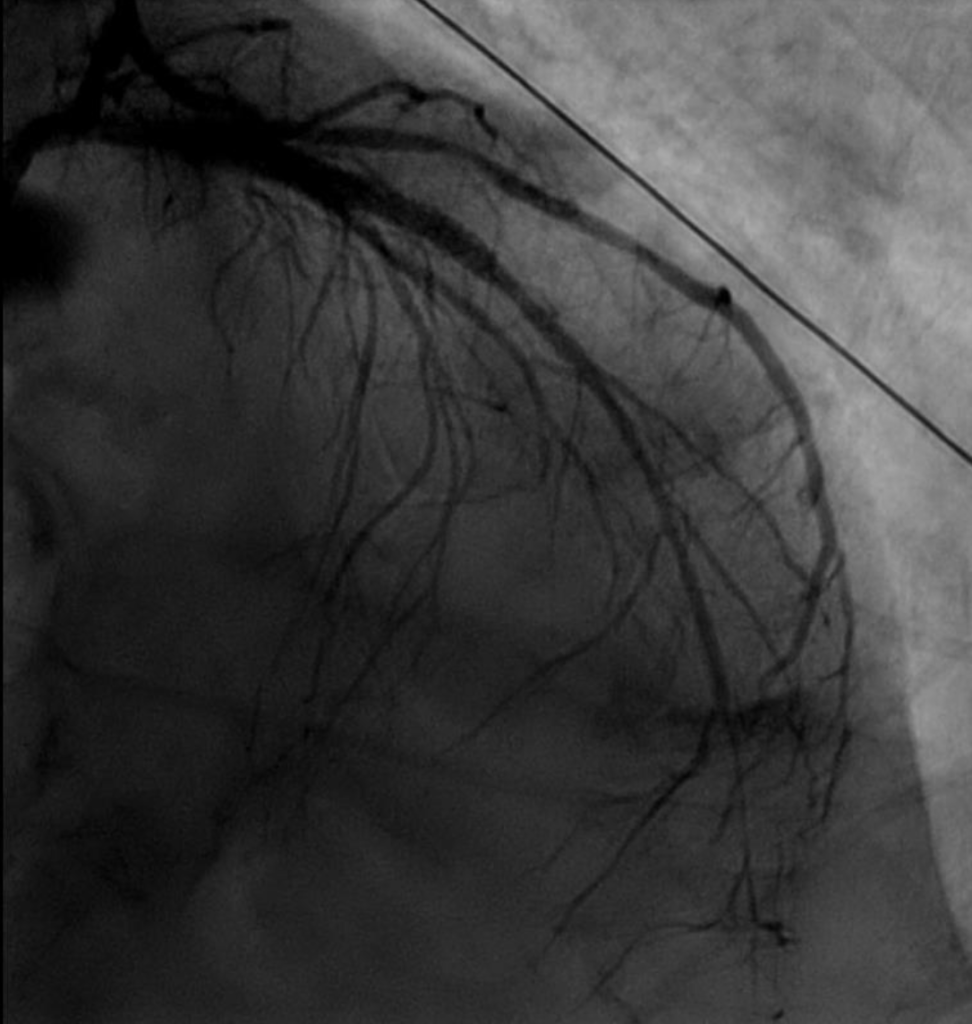
LAD artery post-stenting 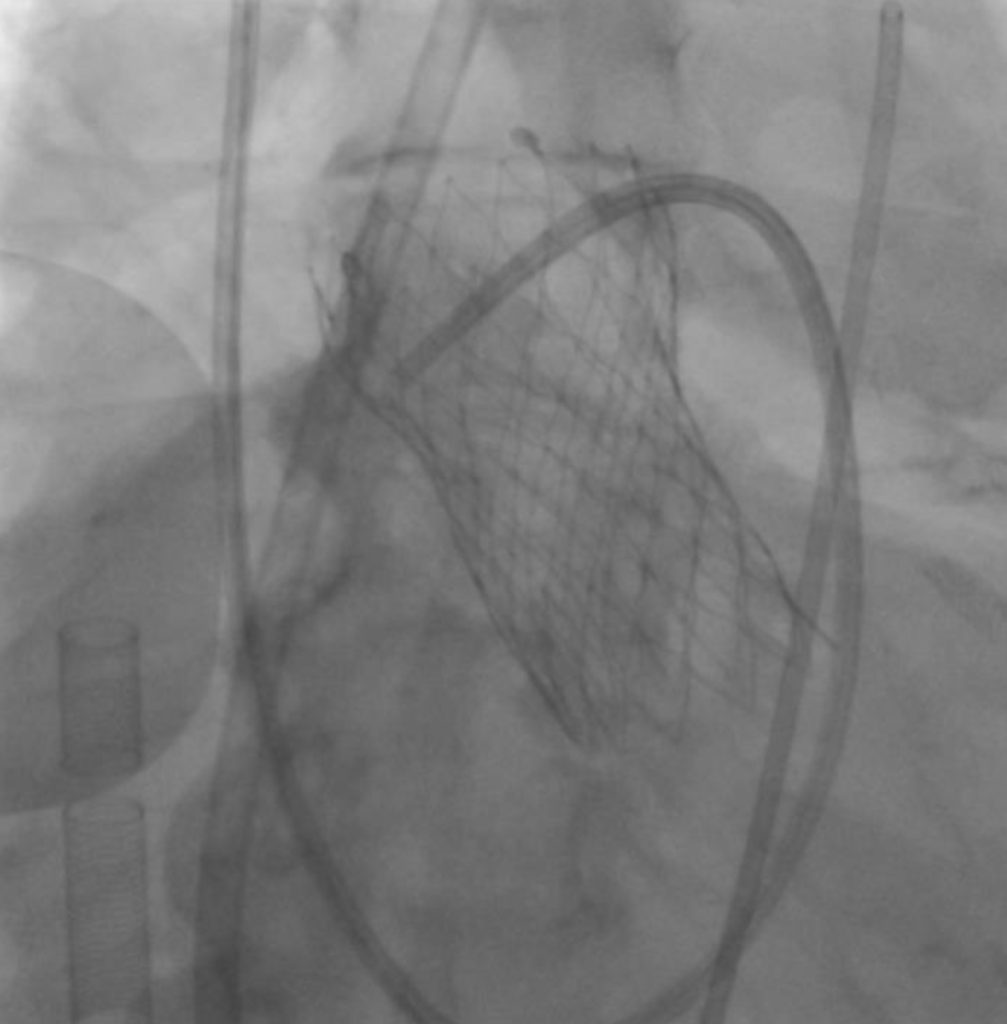
Transcatheter aortic valve replacement (TAVR)
Outcome: Normal Heart Function
The patient spent four days on ECMO after surgery to give the heart time to fully heal. After a lengthy recovery that included cardiac rehabilitation, his heart muscle function improved from a very low ejection fraction back to normal. Now, nine months out from surgery, the patient continues to work on reconditioning to restore his muscle strength. “He is enjoying being back home with his wife, who was with him every step of the way,” says Dr. Sodhi.
“For me, to be able to perform a procedure with immediate, life-saving benefits is the reason I chose my subspecialty of structural and interventional cardiology,” she adds. “To be able to help a patient and get them back to their lives is just so gratifying. His story is why I do what I do and why I chose to become a physician.”
An Atypical Case
This patient was unique in many ways. Most significantly, he is one of the oldest patients to survive this series of complex treatments.
He was also new to the Charlottesville area, so he did not have a primary care provider, leaving Dr. Sodhi without one of the key players she’s accustomed to having involved in her patients’ care. “Typically, we look to the referring doctor for guidance because they know the patient and family very well and have established a relationship with them,” she says. “It’s important to have the referring provider involved in the decision-making process, whether to proceed with a particular procedure and, once the procedure is done, to again circle back and let them know how things went. This ensures complete continuity of care so that nothing is missed, either before the procedure or after. That’s why I’m committed to keeping the referring team informed every step of the way as they are very much a part of our team as well.”
To refer a patient to the UVA Advanced Cardiac Valve Center, call 434.243.1146.