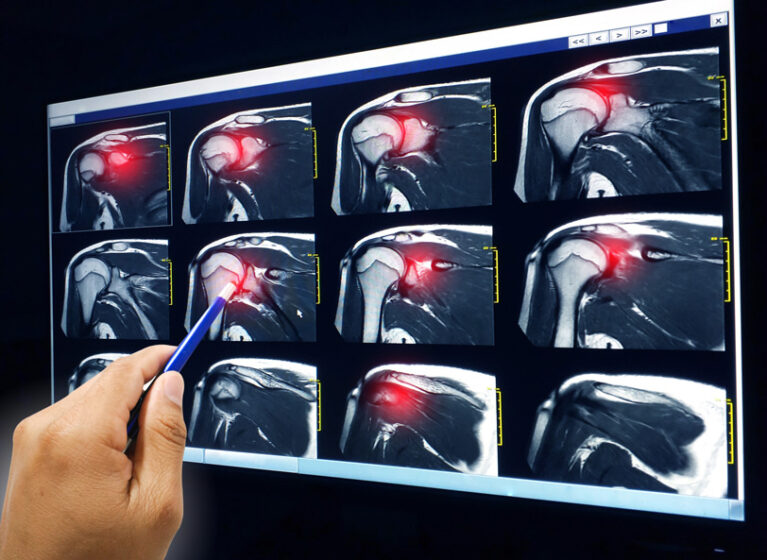
Despite improvements to rotator cuff surgery techniques, many patients still don’t heal properly after surgery. At UVA Health, a team of orthopedic and biomedical engineering specialists is exploring tissue-engineering and regenerative medicine solutions to improve outcomes for this common surgery.
They aim to more completely restore the function of damaged muscles by combining biomaterials, biologicals (i.e., cells or drugs/growth factors), and engineering approaches to optimize and accelerate tissue healing.
They anticipate these approaches will be applicable to a wide range of muscle injuries, such as strains and tears, that cause muscle degeneration and dysfunction.
Creating Preclinical Model to Test Novel Muscle Repair Technologies
To date, research to improve rotator cuff repair has focused on improving bone and tendon healing, including:
- Footprint preparation
- Using platelet-rich plasma, mesenchymal stem cells, or other growth-stimulating techniques
- Improving the biomechanics at the repair site with biologic scaffolds or augmentation techniques
- Improving bone quality at the site of attachment
However, these research avenues don’t address a key component in failed rotator cuff healing: muscle atrophy.
To this end, the UVA Health team has validated a reproducible and biologically relevant small-animal model of rotator cuff repair — with a specific focus on establishing rigorous multiscale metrics for assessing biomechanical mechanisms of muscle damage and repair.
“The unique thing we are looking at within this model is how to optimize it to study rotator cuff muscle atrophy and potential therapeutic interventions to reverse atrophy at the time of repair,” explains Brian Werner, MD, an orthopedic surgeon and researcher specializing in sports medicine and shoulder surgery. This includes metrics such as muscle fiber number, size, location, type, and the extent of fibrosis.
“By optimizing the model and the assessments of atrophy and improvement in muscle characteristics after surgery, it can be used to compare across a diverse array of future potential therapeutics for rotator cuff muscle atrophy — many of which are being developed at UVA Health,” Werner says.
Evaluating Novel Solutions for Numerous Musculoskeletal Indications
The group can now compare the biomechanical basis for muscle damage and muscle repair across multiple length scales — from the molecular lever to muscle fibers, muscle bundles and whole limb movements.
“We have developed multiple preclinical animal models — including the study of both extremity and craniofacial muscles,” says George Christ, PhD, a biomedical engineer. “This provides a very powerful and relatively high throughput preclinical testing platform for screening and evaluating novel and more efficacious solutions for numerous orthopedic and musculoskeletal indications — in this instance, rotator cuff repair.”
Laying Groundwork for Clinical Translation
After identifying successful therapeutics, the team hopes to optimize the technology form factor for use and placement in humans. Their ultimate goal: to give patients the relief they need and get them back to their daily lives.
Clinical translation in humans will require multiple steps. First identifying a successful therapeutic(s), as outlined above. Then the technology form factor would need to be optimized for use and placement in humans, optimally arthroscopically. Lastly, testing in a large animal model, such as a sheep, would be required prior to translating in humans — all while remaining in contact with the FDA for guidance.