Researchers at UVA Health are developing a microporous hydrogel designed to accelerate wound healing and reduce scar formation in the larynx after intubation. Spearheaded by James J. Daniero, MD, associate professor of otolaryngology-head and neck surgery, and Don Griffin, PhD, assistant professor in the Department of Biomedical Engineering, the effort is part of an NIH R-21 research grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Guarding Against Posterior Glottic Stenosis
According to Daniero, about 50% of patients intubated for 3 days or more show signs of acute laryngeal injury (ALgI) after the tube is removed. The vast majority of these patients heal quickly. However, about 5% become acutely and permanently injured, eventually developing posterior glottic stenosis (PGS), a permanently debilitating condition that limits the ability to breathe and requires a tracheotomy.
Patients with diabetes are at particular risk for PGS due to poor glucose control that compromises wound healing. Others at higher risk include critically ill patients with a low tissue perfusion state because medications used to treat shock divert damage-reducing blood flow from nonessential tissue in the larynx to vital organs. Those who are intubated with a larger endotracheal tube (over 7.5 mm for men and 7.0 mm for women) are also at higher risk for ALgI and subsequent PGS.
"We've seen increased incidence of resuscitation sequelae like ALgI throughout the SARS-CoV2 pandemic," Daniero says. "These patients are surviving a life-threatening illness only to leave the hospital with a surgically-implanted breathing tube in their neck for the rest of their lives."
Optimizing the Biomaterial Scaffold
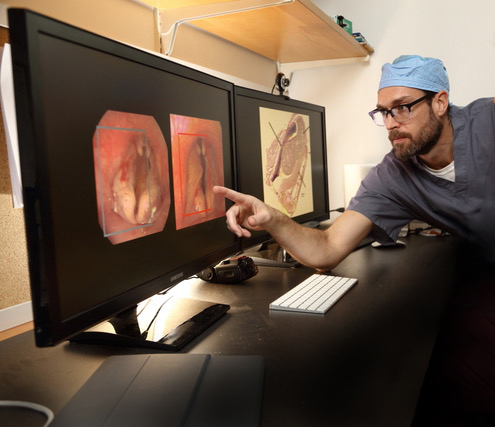
Daniero and Griffin note that the hostile environment of the upper airway is a particularly challenging one for biomaterial-mediated healing. Their novel microporous annealed particle scaffold uses a hydrogel composed of highly concentrated microparticles that are delivered endoscopically to the surface of a mucosal wound and become solidified quickly in situ into a solid scaffold with ~300µm pores. The researchers are optimizing the materials to be heterogeneously decorated with positively charged natural polymers to provide material cohesion and interfacial adhesion for increased material stability.
The first year of the 2-year, NIH-funded project focused on rabbit model development of laryngeal injury and in vitro optimization of the gel's mucosal adhesive properties. This year, the duo will conduct a randomized trial comparing a base hydrogel, the mucosal-adherent hydrogel, and saline to demonstrate wound retention and antifibrotic properties. Their goal is to have the gel adhere long enough for cells to infiltrate the scaffold and lock it into place. This would prevent scarring and limit the tethering of vocal cords into a closed position.
"A key challenge with topical applications in the airway is that the significant mechanical forces of normal airway activity, such as coughing, swallowing, talking, and throat-clearing, can disrupt the integrity of the gel," Daniero explains. "Initial results of our animal study demonstrate that this gel can remain in place for a week without being displaced."
Following completion of the proof-of-concept study, Daniero and Griffin plan to commercialize the final version of the biomucosal sealant for endoscopic wound healing across many applications, including ALgI from COVID-19.
A Fruitful Collaboration in an Ideal Setting
Daniero and Griffin have also collaborated for years to develop and optimize biomaterials to reconstruct the upper airway and larynx. Their first project focused on the development of an injectable biomaterial to reconstruct damaged vocal cords. The current project expands that work into new areas of airway reconstruction.
"We identified an unmet clinical need and are excited that NIH recognizes the importance of developing a novel solution to a serious problem that significantly impacts patients' quality of life," Daniero says. "UVA is an ideal setting for this work because our infrastructure prioritizes fruitful cross-functional collaboration among medical, engineering, and business faculty. That type of collaboration is necessary to translate innovation into marketable products that improve health outcomes."