Although we’re well into 2022, we’re still not close to meeting the goal of 80% by 2018. This widely publicized goal to have 80% of all adults aged 50 or older screened for colorectal cancer was set by the National Colorectal Cancer Roundtable (NCCRT). The COVID pandemic has had a further detrimental effect on colorectal cancer screening. NCCRT estimates that an additional 4,500 lives (or more) will be lost over the next decade that will be attributed to delayed or missed screenings.
“Fully 1/3 of eligible Americans are not up to date with colorectal cancer screening,” says UVA primary care physician Andrew Wolf, MD, chair of the American Cancer Society’s Guideline Development Group. “Redoubling our efforts to promote screening represents a tremendous opportunity to reduce the burden of suffering and death from colorectal cancer, especially since colon cancer screening is one of the most effective things we can do in medicine, both in terms of cost savings and saving lives.”
Colorectal cancer is one of the few that is preventable by screening. “We can estimate that at least 50% of deaths — maybe more — from colorectal cancer are preventable with screening,” says Shari Stanley, RN, nurse administrative coordinator for the UVA Colorectal Cancer Screening Program. “With colorectal cancer, we often have an opportunity to stop it in its tracks before it happens.”
There’s no denying many patients are apprehensive about having a colonoscopy. Others may just be unaware that they should be screened. As providers, we have an opportunity to ensure patients are well informed about why screening is important, when it’s necessary and how it’s done.
Here are 5 points to keep in mind as you discuss colorectal cancer screening with your patients.
Seize Every Opportunity
A patient’s annual preventive visit is a great time to make sure they are up to date on all recommended screenings. However, fewer patients are having yearly check-ups these days. That’s why it’s important to participate in “opportunistic screening,” says Wolf. “Any time I see someone who is overdue for screening, I will raise the issue with them even if they’re there for other medical concerns.”
Another option is to reach out to patients at home. “If you have a good system for recording who is in your practice – an EMR, perhaps – then you might send out reminders to those patients who are out of adherence with screening,” adds Wolf.
There’s no question that the pandemic has had a dramatic impact on colorectal cancer screening, since both primary care office visits and colonoscopies were severely curtailed at the height of the pandemic. Even as we’ve emerged from the worst of it, many folks still want to minimize their interaction with the health care system, making stool-based screening, which is performed at home, a particularly attractive option.
Ask About Family History of Colorectal Cancer
One of the most important questions you can ask your patients is whether they have any family history of colon cancer, Wolf says. “Patients may not offer up that information, so it’s important to ask. A family history of colon cancer or advanced polyps should prompt the provider to recommend earlier screening and they can detect familial cancer syndromes.”
“Having a family history of colon cancer can increase your risk of a diagnosis by as much as four times compared to the average person,” says Stanley. “It’s a greater risk factor than anything else. People tend to focus on modifiable risk factors like smoking, sedentary lifestyle, drinking alcohol – but these things have less of a link to colorectal cancer than family history.”
Colon cancer screening is one of the most effective things we can do in medicine, both in terms of cost savings and saving lives.”
Dr. Andrew Wolf
Don’t Overlook Younger Patients at Risk for Colorectal Cancer
You’re likely aware that more and more young people are being diagnosed with colorectal cancer. An estimated 10.5% of new colorectal cancer cases occur in people younger than 50. Colorectal cancer diagnoses among Americans ages 40 to 49 increased by almost 15% from 2000-02 to 2014-16, according to the U.S. Preventive Services Task Force. Based on those figures, the task force updated its colorectal cancer screening guideline recommendations in May 2021, lowering the age to begin screening to 45.
This change has the potential to save thousands of lives every year in the U.S. Wolf says, “In terms of reducing colon cancer — both incidence and mortality — we need to make sure folks get screened no later than age 50, as opposed to age 55 or 60. This is one of the major areas we could improve upon.”
Of course, patients who have a family history may begin screening even sooner. “The age patients should begin screening depends on how many family members they have with a history of colon cancer and what ages they were diagnosed,” says Stanley. “In general, the recommendations are to start screening 10 years before the first-degree family member was diagnosed.”
So, if a patient’s brother was diagnosed at age 50, he would want to start screening at age 40. If he’s had more than one family member diagnosed, he may want to begin even earlier.
Educate Patients on Colorectal Cancer Screening Options
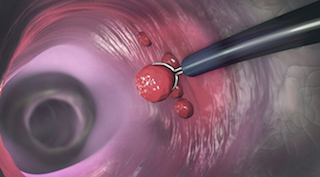
Colonoscopy is still the gold standard for detecting colon cancer because it is the only test that can clearly identify and remove precancerous polyps. Plus, the test is so thorough that results are valid for 10 years. However, there are some drawbacks that make patients wary of the testing.
“Colonoscopy requires patients to prep by taking a powerful laxative overnight. Then they must take a whole day off work, and they require transportation because they get a sedative,” says Wolf. It’s important to address the pros and the cons and offer the patient a choice.
If colonoscopy isn’t preferred, there are good alternatives. “We could easily extend our screening rates up to 80% if we did a better job of offering options to patients, specifically at-home options,” says Wolf.
There are two at-home testing options that look for traces of blood in the stool, an indication polyps may be present. These stool-based tests are easier for patients. Yet, they must be done more frequently and, if results are positive, the patient still must have a colonoscopy to confirm a diagnosis.
UVA switched to Polymedco® FIT that finds more colon cancers without significantly increasing the false-positive rate
- FIT Test (fecal immunochemical test)
The FIT test looks for microscopic blood in the stool. Providers may keep this test on hand in their office, which makes it easy to provide patients instructions for use and answer any questions they may have. Patients do the test at home and send samples back to the lab. As results come back, they are entered directly into the patient’s record if the provider uses an EMR. A FIT test must be repeated annually. We’re very excited to announce that UVA switched our FIT test to Polymedco® FIT this month. The new FIT offers significantly greater sensitivity – finding more colon cancers – without significantly increasing the false-positive rate. This makes FIT an even more attractive option for individuals going forward. - Cologuard®
This test is the same premise as the FIT test, although it looks for DNA mutations in addition to blood in the stool that may signal the presence of polyps or colorectal cancer. To order this test, a provider must submit a form to the company, which will then send the test to the patient. This test must be repeated every three years.
Additional colorectal screening options include:
- CT Colonography
This “virtual colonoscopy” is a screening method that uses a series of x-rays to scan the colon and rectum, so it’s less invasive than colonoscopy. Patients still have to prep for the test, yet there is no sedation required. Often they can head back to work immediately after. If results are normal, the patient won’t need to be screened again for five years. Because this test is fairly new, insurance may not cover it.
- Flexible Sigmoidoscopy
Less commonly used today, the flexible sigmoidoscopy is similar to a colonoscopy, however the screening only covers the lower portion of the colon. Patients are required to prep prior to the test, yet they are not sedated, so it’s less involved. The results are good for five years.
Consider Insurance Coverage
Since both ACS and USPSTF recommend starting screening at age 45, most insurance companies have followed suit and lowered the starting age of coverage to 45. This should help tremendously with uptake of the new recommendation.
Despite the recommendations to begin screening at age 45, not all insurance companies are on board with the change. That’s why it’s best to encourage all patients to reach out to their insurance provider to confirm coverage prior to the test just in case.
Another thing to keep in mind as we introduce at-home and other alternative screening options: a colonoscopy likely will be necessary to confirm a diagnosis if the initial screening comes back positive. Recent legislation should have a positive impact on commercial insurance coverage for the follow-up colonoscopy. The intent of the legislation is to treat the follow-up colonoscopy as part of the fully covered screening cascade for colorectal cancer.
“There is lots of lobbying at the state and federal level to make that follow-up colonoscopy part of the screening,” says Wolf. “We should be thinking of the at-home test and colonoscopy as a two-step process, but for now, patients should ask their insurance providers about coverage.”
BOTTOM LINE: The best colorectal cancer screening test is the one that gets done!
Learn more about the insurance considerations for colorectal cancer screening.
UVA Cancer Center and VCU Massey Cancer Center have teamed up to boost from 70.8 to 80% the percentage of Virginians up to date on their colorectal cancer screenings. Learn more about this partnership.