At a Glance
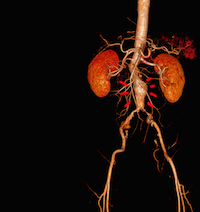
- A majority of abdominal aortic aneurysms are treated using stents and a minimally invasive approach.
- Despite the benefits of endovascular aneurysm repair, we now know that this isn’t the best long-term option for all patients.
- The rate of certain aneurysm-related complications that occur years after endovascular AAA surgery is higher compared to open surgery.
- UVA vascular surgeons are skilled at treating endoleaks and other complications.
More and more operations today are being performed using minimally invasive techniques. Abdominal aortic aneurysm repair is no exception.
“Over the past decade, we’ve seen a transition. Now, because of significant advances in surgical technologies, a majority of aneurysms are treated using stents and a minimally invasive approach,” says UVA vascular surgeon Megan Tracci, MD. “Aneurysm repair is now an overnight stay in most cases, as opposed to the 3- to 5-day postoperative hospital stay traditionally required for open surgical repair.”
The advantages of an endovascular aneurysm repair (EVAR) extend beyond just length of stay, of course. There is less pain and a shorter recovery time. Most importantly, mortality and serious complication rates at the time of surgery also are much lower.
“Studies have shown that there is a 1.6% perioperative 30-day mortality for endovascular aneurysm repair compared to up to 5% mortality for open surgery,” says Tracci. “Open aneurysm repair is a big operation, so you have all of the risks that come with that, including heart attack and pneumonia. That’s why – for both the patient and physician – endovascular repair with stents often is more appealing.”
A Fresh Take On the Long-Term Advantages of EVAR
Despite the benefits of a minimally invasive approach to elective AAA repair, we now know that EVAR is not the best long-term option for every patient. Recent research shows that the survival advantage you might get initially with endovascular repair doesn’t always stand the test of time.
“Studies show the survival advantage we see with EVAR disappears at around five years,” says Tracci. “This is likely for a variety of reasons, but one thing that we do see is that the rate of certain aneurysm-related complications that occur years after endovascular AAA surgery is higher compared to open surgery. There’s a higher rate of re-intervention; people often need subsequent procedures to tune things up.”
AAA: Post-Repair Complications
One of the most common complications after EVAR is an endoleak or the continued flow of blood to the aneurysm sac, which puts the patient at ongoing risk for rupture. “Often, little branch vessels continue to feed into the aneurysm, so we have to find a way to stop that blood flow,” says Tracci.
The treatment varies from patient to patient depending on the type of endoleak, but typically the go-to fix is another endovascular procedure, either inserting a new graft or transcatheter embolization to block feeding vessels. The question is: how many endovascular procedures are too many?
“We’re finding that some people who have undergone repeat endovascular attempts to treat endoleak are requiring either bigger procedures or open interventions during which we actually go in and tie vessels off surgically or take a graft out and replace it with a surgical graft.”
UVA has become a regional referral center for endoleaks and other AAA repair complications because its team has the skill and experience to offer the procedure that is best for each individual patient. “When you refer to us, you can have confidence that we are able to treat patients based on their unique needs,” says Tracci. “We can put all of the treatment options on the table. We have a multidisciplinary team skilled at treating the entire aorta from the heart to the legs, including those requiring cardiopulmonary bypass — so we can do the full spectrum of surgery.”
The Right Choice from the Start
Of course, the best way to manage complications of aneurysm repair is to prevent them. At UVA, surgeons help mitigate the risk of complications on the front end by choosing the right aneurysm fix from the start. This requires vascular surgeons to take a careful look at the patient’s anatomy and comorbidities to help choose the right approach for each individual.
“For some patients, open repair up front may be a better option,” says Tracci. “We weigh each case individually and share the decision-making with the patient. We do quite a bit of open aortic surgery and are comfortable that we’re offering them state-of-the-art care no matter what they choose.”
Who to Refer
Patients Who Have Had a Previous EVAR
As with unruptured aneurysms, there are generally no symptoms associated with endoleak. If you have a patient who had an EVAR in the past, regular imaging is required to monitor for complications, such as filling or growth of the residual aneurysm sac outside the graft. Should routine imaging reveal signs of a complication, refer your patient to specialists like those at UVA who are experienced managing these conditions and providing the full spectrum of repeat aneurysm repair procedures.
Patients Whose Screening Results Are Positive for AAA
As you know, AAA is much more likely to be fatal if it ruptures. The sooner you refer for a consult with a vascular surgeon, the better your patient’s chances of survival. At UVA, heart and vascular specialists carefully assess each patient to determine the next best steps in terms of risk factor modification, surveillance and treatment should an aneurysm be identified. Every patient has access to the resources they need to manage their condition effectively, whether they choose to enroll in a smoking cessation program, make lifestyle changes or receive medication to address high blood pressure or other risk factors, or undergo an elective aneurysm repair.
An Update on AAA Screening
Ruptured abdominal aortic aneurysm remains the 15th leading cause of death in the U.S. According to a study published in the Journal of Vascular Surgery in 2017, approximately 43% of fatal AAAs occurred in people not eligible for screening under past guidelines; many of them were women. A renewed focus on more comprehensive screening has the potential to alter that statistic.
At UVA, the heart and vascular team follows the more current AAA screening guidelines recommended by the Society for Vascular Surgeons. Tracci says she and her team are particularly vigilant when it comes to assessing women at increased risk for AAA.
“The U.S. Preventive Services Task Force came out with initial screening guidelines in 2005 that did not recommend screening for women. I believe that was because so few women were involved in trials that they were not statistically able to identify a decrease in mortality with screening,” she says. “I am one of those surgeons who believes we ought to be very thoughtful about screening women for aneurysm. Although these occur less frequently in women, we know the rate of rupture is higher and life expectancy is higher.”
For all patients over age 65, screening for AAA should be a consideration. “The study is minimally invasive with no radiation. It’s relatively quick and inexpensive using an abdominal ultrasound,” says Tracci. “Patients may be screened through the program at UVA or the test can be ordered by a patient’s primary care provider. It’s also now covered by Medicare.”
Learn more about vascular screening at UVA.
To refer a patient to UVA Health, call UVA Physician Direct at 800.552.3723.