
At a Glance:
- Skin cancer can occur around the eye, but melanoma in this location is rare
- Excising cancer from the eyelid requires skill and precision to retain both functionality and appearance
- Collaboration among providers from dermatopathology, dermatologic surgery and ophthalmology ensures the best outcome for the patient
The common treatment for melanoma in situ, or melanoma confined to the outer layers of skin, is surgical excision. However, this standard approach becomes much more complicated when melanoma appears on the delicate tissue surrounding the eye.
To ensure the best outcomes, in terms of both disease eradication and preserving the appearance and functionality of the eye, UVA Health takes a collaborative approach to treatment that brings together skilled providers from dermatopathology, dermatologic surgery and ophthalmology. The case study below demonstrates why these specialists are among the best in their field.
Case Study
Patient: 52-year-old male
Evaluated by: Maria Kirzhner, MD; Mark Russell, MD; Mark Wick, MD
Diagnosis: Lower eyelid melanoma in situ
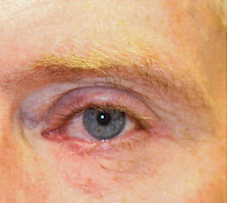
The patient had a non-suspicious freckle present on his left lower eyelid for one year. At his annual follow-up visit, ophthalmologist Maria Kirzhner, MD, noted that the lesion was not improving and had persistent redness surrounding it. “I recommended a biopsy of the lesion to check for any malignant cells due to the persistent redness of the lesion and the patient’s high risk characteristics: blonde-haired, blue eyes and a history of skin burns,” says Kirzhner.
A sample from the biopsy was submitted to UVA Health dermatopathologist Mark Wick, MD, who confirmed a diagnosis of melanoma in situ. “Skin cancers can occur around the eye, but melanoma is not one of the more common ones,” says dermatologist Mark Russell, MD.
Treatment: Excision followed by reconstruction

With a confirmed diagnosis, Kirzhner referred the patient to Russell for surgery to remove the cancerous cells. “This patient’s skin cancer was small and relatively thin, so we could remove it using standard surgical technique and routine pathology lab evaluation,” says Russell. “Other surgical techniques, including Mohs surgery, can be used depending on the situation. We treat every lesion and every person individually, considering all relevant variables to come up with the best treatment that will ensure the best outcome for each patient.”

During the outpatient procedure, the patient was given local anesthesia to numb the eyelid. His eye was sufficiently protected using an eye shield. Russell excised the lesion and a margin of normal-appearing skin around it, removing about one-third of the lower left eyelid. “My job is to remove the cancer completely with as little collateral damage as possible,” he says. This tissue was sent off to pathology to confirm the margins were clear, signaling that all cancer was removed.
“We were able to close up the incision and send the patient on to Dr. Kirzhner with good confidence of clear surgical margins so that she could then finish the repair,” says Russell. “He had
reasonable functionality of his eyelid at that point.”
The patient returned to Kirzhner a few days later to complete the eyelid repair. He was put under conscious sedation during the half-hour procedure. “With his tissue and the size of the defect, it was appropriate to move some nearby local remaining eyelid around to recreate a new, normal functioning eyelid edge. But we didn’t have to do anything aggressive,” says Kirzhner. “The most important thing for eyelid reconstruction is that the eyeball is covered, that the lid moves up and down, that there’s no tension – it’s not too tight, but not droopy. His surgery went exceptionally well.”
“Given the delicate nature of the eyelid, I was so fortunate Dr. Kirzhner had the expertise to do a less-invasive procedure to make my recovery so much easier,” the patient says.
Recovery: antibiotic cream, ice and follow up
Bruising and swelling are commonly associated with any eyelid procedures and can persist for up to two weeks or more, according to Kirzhner. This patient used ice compresses for two days to decrease swelling and bruising, and he took acetaminophen as needed for discomfort. He applied an antibiotic ointment at the site of incision to help with healing twice per day. He returned for follow up with Kirzhner to remove sutures two weeks later.
Today, his eye is completely healed, fully functional and normal in appearance. “It’s amazing to know where we started and to see the minimal scarring he has now,” says Russell.
“This experience got my attention,” the patient says. “I will be advocating for better sun protection among my friends and teaching my son about skin cancer prevention. Everyone needs to be aware of ways to prevent melanoma so that special procedures like this don’t need to be performed. But I was blessed to be at UVA where a team of experts could completely remove the cancer from this delicate area.”
Signs of Malignant Neoplasm on the Eyelid
Here are some of the most common signs of malignancy to look out for in your patients:
- Spots that are growing and not resolving
- Eyelash loss
- Discharge, especially bleeding
- Scabbing around the lesion
- Any change in color
- Non-resolving eye irritation.